According to Diabetes.org.uk, around 4.9 million people in the UK are living with diabetes. Worryingly, this number is growing fast with figures also suggesting 5.5 million UK people could have the condition by the year 2030.
Despite being fairly common, diabetes is also dangerous. Over time, high blood glucose levels can damage the body’s organs and blood vessels. This in turn increases the chance of a heart attack or stroke, as well as problems with the eyes, kidneys, gums, nerves, legs and feet.
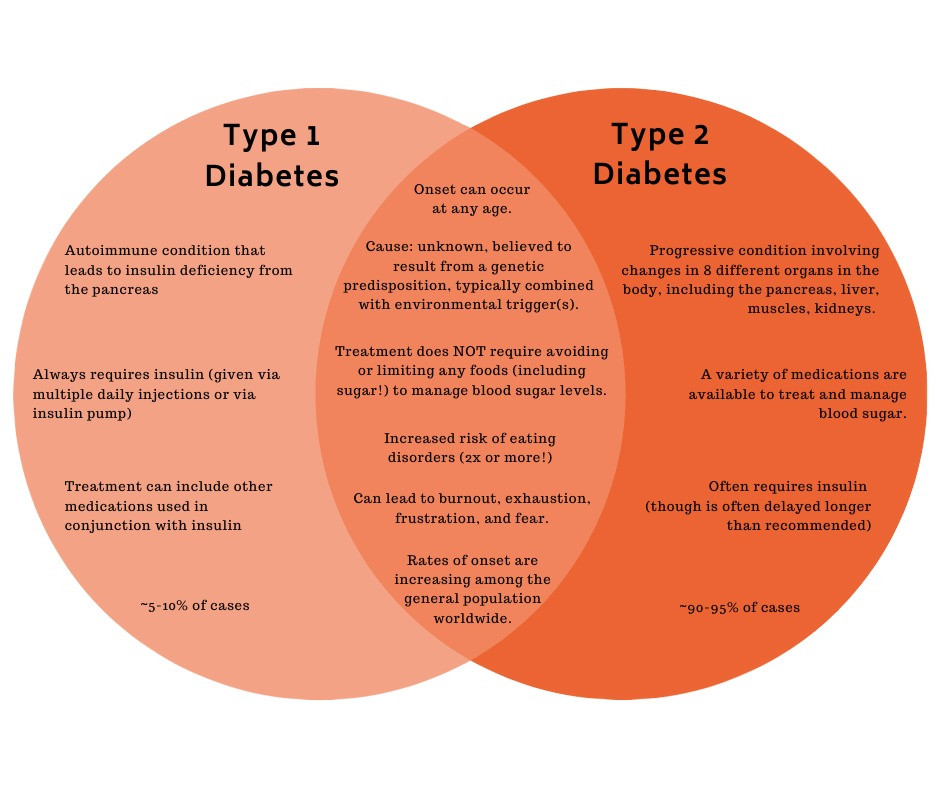
It’s down to healthcare practitioners to spot the signs early, and understand the key differences between type 1 diabetes and type 2 for optimum management.
Type 1 diabetes
Type 1 diabetes can affect patients of any age. However, it’s most commonly detected in people between infancy and 40 years old.
With type 1 diabetes, the pancreas does not make insulin required to meet the body’s needs. Scientists are still unsure why it happens, but type 1 diabetes occurs when the immune system attacks and destroys insulin-producing cells.
The only treatment for type 1 diabetes is insulin. This is usually infused via a pump, or injected.
Type 2 diabetes
Type 2 diabetes is far more common in the UK than type 1. In fact, of all those diagnosed with the condition, the vast majority – around 90% – have type 2. It also usually affects those over 40, or 25 in those of South Asian descent. Having said that, more and more younger people are presenting with the condition.
The symptoms of type 2 diabetes are often not obvious. They can also develop over a much longer period of time (unlike type 1).
Patients with type 2 diabetes either don’t make enough insulin or don’t make insulin that can be used effectively by the body. Their cells start to become resistant to insulin, meaning the pancreas has to make even more of it to try and maintain glucose levels within a normal range. This excessive insulin production, paired with ever-fluctuating insulin levels, mean over time the pancreas becomes damaged. It may then start to fail, producing less and less insulin so that the patient requires medical intervention.
Unlike type 1, type 2 can in fact be reversible via an effective diet and exercise. Patients must also maintain their health by self-monitoring their blood glucose. However, type 2 diabetes is typically a progressive condition, meaning that most patients will require tablets and/or insulin injections after living with the condition for five to 10 years.
Would you like to increase your professional knowledge around diabetes management?
Designed specifically for healthcare assistants and support workers, PDUK’s Diabetes basics for HCAs course is ideal for those who regularly see diabetic patients. An interactive 1-day online course worth 7 hours of CPD, it gives HCAs in primary and secondary care a basic understanding of diabetes, boosting confidence in managing patients with the condition. All levels of HCA knowledge and skills are accommodated, and it’s a great way to network with others in your field.
Why not take a look at the course details and sign up today. Spaces are always limited so secure yours soon to avoid disappointment.